De novo genetic variant in epileptic encephalopathy: Importance of specific diagnosis


Authors
DOI:
https://doi.org/10.37980/im.journal.ggcl.20242381Keywords:
early infantil epileptic encephalophathy, CYFIP2 gene, whole exome sequencing, precision medicineAbstract
Introduction: Early infantile epileptic encephalopathies (EIEE) are rare syndromes that affect neurological development. The etiology has been uncertain for a long time, but advances in genetics have identified numerous associated genes. Variants in the CYFIP2 gene have been linked to EIEE.
Clinical case: An 11-year-old female born at term without complications, with microcephaly, synophrys, and short neck. No relevant family history. At one month, she developed generalized seizures and delayed neurodevelopment, progressing to severe spastic quadriparesis, requiring gastrostomy and tracheostomy, with paroxysmal discharges on electroencephalogram. She received multiple anticonvulsant medications and ketogenic therapy. Complete individual exome sequencing and analysis of deletions and duplications were requested. Individual complete exome + deletions and duplications analysis (CNV) identified a probably pathogenic heterozygous variant in the CYFIP2 gene variant c.259C>T (p.Arg87Cys) missense type, allelic ratio (VAF) 0.45. The results of this molecular study support the diagnosis of developmental and epileptic encephalopathy de novo.
Discussion: Developmental and epileptic encephalopathy (EED) disorders are severe conditions that begin in childhood, characterized by epileptic seizures, abnormalities in the electroencephalogram, and deterioration of neurodevelopment. Genetic EEDs are associated with variants in various genes related to cellular and neuronal functions. The CYFIP2 gene, on chromosome 5q33.3, encodes protein 2 that interacts with FMRP (fragile X mental retardation protein), playing a crucial role in neurological development. De novo variants, such as nonsense mutations and truncation in CYFIP2, are associated with intellectual disability, seizures, and muscle hypotonia. Advancements in genomics are improving the understanding of epilepsy, impacting targeted treatment, prognosis, and patient counseling. Childhood epilepsy has a heterogeneous genetic basis, and some patients without previous diagnosis can now receive one, crucial for the implementation of precision medicine.
Introduction
Intellectual disability is a genetically heterogeneous disorder with a prevalence of 2 to 3%, and epilepsy is a common comorbidity. Genetic defects are believed to be a significant cause of these pathologies, but identifying causal variants is complicated by considerable genetic heterogeneity [1]. Early infantile epileptic encephalopathies (EIEE) are a rare group of neurodevelopmental syndromes that appear in early childhood. In this pathology, seizures and epileptic episodes hinder proper neuronal development. The precise incidence of this set of syndromes is not reported. However, it is estimated that infantile spasm syndromes (or West syndrome), which are also included within EIEE, have an incidence of approximately 0.25 cases per 1,000 live births. Its prevalence is around 1 in 10,000 children aged 10 years [2].
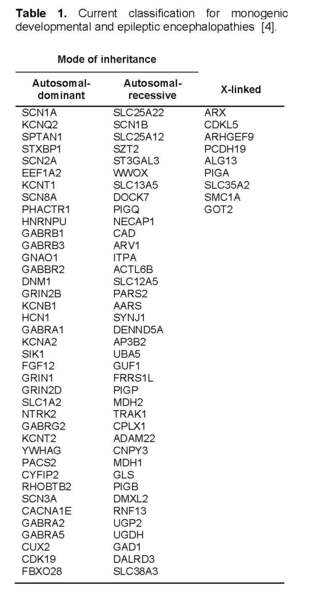
For a long time, the etiology of severe infant-onset epilepsies remained uncertain, and most were attributed to acquired causes. In the last two decades, advances in molecular genetics have allowed the identification of nearly a hundred genes associated with what are now known as epileptic and developmental encephalopathies [3].
The diagnosis of EIEE remains a challenge, and next-generation sequencing (NGS) techniques have played a crucial role in identifying monogenic causes. Recent studies have shown an association between variants in the CYFIP2 gene and early infantile epileptic encephalopathy [5].
Case Report
Female patient, 11 years old, born from the fifth pregnancy, with a 35-year-old mother and a 30-year-old father (age at conception). The birth was full-term without complications at 40 weeks of gestation, with no prenatal ultrasound abnormalities, appropriate birth weight, and no height data at birth. The patient had a history of neonatal jaundice managed with phototherapy. There was no family history of consanguinity, diseases, or congenital malformations.
On physical examination, the patient presented with microcephaly, synophrys, almond-shaped eyes, high-set ears, and a short neck. At one month of age, she began experiencing seizure episodes during sleep and wakefulness, presenting with bilateral right ocular version and generalized tonic flexion posture lasting for seconds. These episodes were persistent, occurring more than 10 times a day, associated with delays in developmental milestones, and failure to achieve higher brain functions. She evolved to GMFCS (Gross Motor Function Classification System) IV spastic quadriparesis, underwent gastrostomy at 6 months old, and required tracheostomy with mechanical ventilation since 18 months of age.
Paraclinical studies were performed to rule out inborn errors of metabolism and mitochondrial disorders, including measurements of blood lactate and pyruvate, blood ammonia, serum and urine amino acids, carnitine levels and blood acylcarnitine profile, which were normal. An electroencephalogram showed baseline activity characterized by an 8 Hz posterior Alpha rhythm, reactive, symmetrical, and an anterior Beta rhythm of more than 18 Hz with an amplitude below 20 µV, interspersed with muscle-origin activity and some slow activities in the lateral regions, photostimulation at frequencies between 5 and 30 Hz did not produce significant alterations, no interictal activity was observed during the recording, ictal activity throughout the tracing showed paroxysmal discharges of sharp waves in the right frontoparietal regions with contralateral irradiation. Therapeutic indications included lamotrigine, clobazam, vigabatrin, clonazepam, risperidone, and levomepromazine, but the episodes were not controlled, besides the patient exhibited self-injurious and hetero-aggressive behaviors, leading to the initiation of ketogenic therapy, which improved seizure frequency. Considering the clinical evolution, complexity, and neurobehavioral characteristics with a high suspicion of a genetic origin, whole exome sequencing plus deletion and duplication analysis (CNV - copy number variant analysis) was requested.
A whole exome sequencing (covering the entire coding region of the genome and intron-exon junction regions, corresponding to approximately 23,000 nuclear genes) was performed by a third-party provider Gencell, using a next-generation sequencer DNB-SEQ400 with an MGI-V5 exome library. Subsequently, the identified variants in genes with known clinical associations and related to monogenic diseases were analyzed in relation to the patient's phenotype and described clinical manifestations. The genes were analyzed with an average coverage exceeding 98% and a minimum depth of 20x. The sequencing results were bioinformatically analyzed through a secondary analysis to evaluate the quality of the sequencing data and a tertiary analysis to align the sequences, call and filter variants, meeting specific quality criteria. The variants were analyzed against the hg19 reference genome for annotation and variant calling. The analysis was aimed at identifying variants in exonic regions or splicing regions (at least 20 bp), small insertions and deletions, located in genes related to the patient's clinical phenotype. Parameters such as the population frequency of the variant (ExAC, gnomAD, 1000 Genomes), its allelic ratio, the phenotype associated with OMIM, its classification in ClinVar, and the inheritance method were used to filter the variants to be reported. This analysis allows the identification of exonic deletions and duplications (Copy Number Variants, or CNVs) and variants involving large regions of the gene, which will be reported. The identified variants were evaluated considering the parameters recommended by the American College of Medical Genetics (ACMG) guidelines for variant classification (Richards et al., 2015) and their updates according to ClinGen (clinicalgenome.org), including information from databases such as ClinVar, HGMD, LOVD, dbSNP, and gnomAD v4.1.0.

The individual whole exome sequencing plus deletion and duplication (CNV) analysis identified a likely pathogenic heterozygous variant in the CYFIP2 gene (NM_001037333.3), variant c.259C>T (p.Arg87Cys), a missense type, with an allelic fraction (VAF) of 0.45. This variant could support the diagnosis of developmental and epileptic encephalopathy 65 with autosomal dominant inheritance. The results of this molecular study support the diagnosis of de novo developmental and epileptic encephalopathy 65, given the lack of related personal and family history.
Discussion
Developmental and epileptic encephalopathies (DEEs) are a heterogeneous group of disorders characterized by early-onset epileptic seizures, often severe, and abnormalities on electroencephalogram in a context of developmental regression that tends to worsen as a consequence of epilepsy. Genetic DEEs have been associated with variants in many genes involved in various functions, including cellular migration, proliferation, and organization, neuronal excitability, and synaptic transmission and plasticity [6].
The dynamics of the actin cytoskeleton are critically involved in various aspects of neuronal development and function, including early migration, dendritic and axonal growth and branching, and synapse formation and plasticity. Consistently, several variants of genes encoding key regulators of the neuronal actin cytoskeleton have been associated with numerous neuropsychiatric and neurodevelopmental disorders, such as autism spectrum disorders, intellectual disability, schizophrenia, and bipolar disorder. Among the key regulators, the WAVE regulatory complex (WRC) is a ~400 kDa heteropentameric protein complex consisting of the Wiskott-Aldrich syndrome protein family, WAVE homologous to verprolin, cytoplasmic FMR1-interacting protein (CYFIP), Nck-associated protein (NAP), Abelson-interacting protein (ABI), and hematopoietic stem cell-specific protein (HSPC300) [7].
The CYFIP2 gene is located on chromosome 5q33.3 and encodes the cytoplasmic FMRP interacting protein 2 (CYFIP2). It is believed to play a significant role in neurological development by linking FMRP-dependent local transcription to signaling-dependent cytoskeletal remodeling as part of the WAVE regulatory complex (WRC). The WRC is a key regulator of actin dynamics and is formed by WASF (also known as WAVE), CYFIP1/2, NCKAP1, ABI, and BRICK1 (or their homologs). In the basal state, CYFIP intrinsically inhibits the heteropentameric WRC by sequestering the VCA domain of WASF, which carries activity. Binding of the small GTPase RAC1 to CYFIP induces conformational changes in the WRC, releasing the VCA domain to trigger Arp2/3-induced actin polymerization at various membrane sites. Consequently, the WRC signaling pathway plays a crucial role in important neurological developmental processes, such as axon guidance and regulation of synaptic morphology [8].
Unlike CYFIP1, the neuronal function and dysfunction of CYFIP2 remain largely unknown, possibly due to the relatively less established association between CYFIP2 and brain disorders so far. However, despite the high sequence homology between CYFIP1 and CYFIP2, several lines of evidence suggest they may have distinct functions in vivo. Additionally, recent whole exome sequencing (WES) studies have identified de novo variants at hotspots in CYFIP2 in patients with early infantile epileptic encephalopathy (EIEE) [7]. De novo nonsense variants affecting a small number of amino acids and a late truncation variant in CYFIP2 have been associated with intellectual disability, seizures, and muscle hypotonia [8].
In 2018, Nakashima et al. identified three de novo nonsense variants at residue Arg87 that caused gain-of-function effects in the Wiskott-Aldrich syndrome protein family (WAVE) signaling pathway in four unrelated individuals with early infantile epileptic encephalopathy (EIEE). All individuals experienced intractable seizures (since six months of age) and severe psychomotor developmental delay, associated with other common features such as microcephaly, facial dysmorphism, and hypotonia. Initial interictal electroencephalograms showed burst suppression and/or hypsarrhythmia patterns, consistent with Ohtahara syndrome and West syndrome, respectively. Brain magnetic resonance imaging revealed diffuse cerebral atrophy in all three individuals, primarily in the frontal lobes [9].
In 2019, Zweier et al. reported on 12 patients carrying a total of eight different de novo variants in CYFIP2 with a shared phenotype of intellectual disability, seizures, and hypotonia. Shared morphological characteristics among the patients included high forehead, narrow and slightly up-slanting palpebral fissures, apparent hypertelorism, bulbous nasal tip, full cheeks, everted vermilion of the lips, and retrognathia. Most patients exhibited generalized or truncal hypotonia, limb spasticity, visual impairment, and/or strabismus. Brain magnetic resonance imaging revealed nonspecific structural abnormalities ranging from atrophy to hypomyelination. Epilepsy was intractable in 6 out of 12 patients, and various seizure types were reported, including absence, myoclonic, generalized tonic or tonic-clonic, and epileptic spasms. Electroencephalogram findings included variable epileptiform discharges, including focal, multifocal, and generalized, as well as burst suppression and hypsarrhythmia [10].
In this clinical case, we observe a patient who develops numerous seizure episodes from one month of age, which are difficult to manage, with deterioration in neurodevelopment, leading to spastic quadriparesis. She requires a combination of anticonvulsant medications, including ketogenic therapy, and psychotropic medication. The electroencephalogram results show ictal activity throughout the tracing with paroxysmal discharges of sharp waves in the right frontoparietal regions with contralateral irradiation. Molecular confirmation of genetic origin, specifically developmental and epileptic encephalopathy 65, is achieved through the identification of a likely pathogenic heterozygous variant in the CYFIP2 gene, inherited in an autosomal dominant manner, in a patient with no related family history, suggesting de novo variant.
Recent technological advances, including next-generation complete exome sequencing, have identified many variants. Due to ongoing diagnoses and the mapping of genetic profiles, the number of genes implicated in this pathology continues to grow continuously [11].
It is important to take into consideration, most severe epilepsies result from de novo mutations, with a low recurrence risk due to germline mosaicism when parents are unaffected (estimated to be about 1%). The possibility of parental somatic mosaicism in apparent de novo variants have also to be considered, with reported figures up to 10% of families. The resulting recurrence risk cannot be calculated, but can approach 50% as observed in autosomal dominant disorders. Familial clustering can also result from parental transmission with classical mendelian inheritance, especially for genes with variable penetrance and expressivity [12].
Preclinical and clinical studies suggest that the ketogenic diet (KD), high in fats and low in carbohydrates, effectively controls drug-resistant seizures. Evidence has also shown some efficacy in improving cognitive abilities. A better understanding of the molecular mechanisms through which the KD and new anticonvulsant medications may alleviate seizures and cognitive deficits is crucial for developing new drugs with overall efficacy while minimizing side effects as much as possible. Animal models are well-suited for this purpose; they offer the advantage of studying pathways relevant to disease pathology, as often the primary target (i.e., a defective gene and encoded protein) is not pharmacological [13].
The quest for an effective treatment for various forms of epileptic encephalopathy is a priority for science and society. In recent years, a push towards precision medicine using novel anticonvulsant drug candidates and targeted gene therapy has emerged as a viable treatment strategy for different diseases and holds great promise for drug-resistant epilepsies. More preclinical studies in children suffering from drug-resistant seizures are needed. Considering the variability and phenotypic pleiotropy typical of epileptic encephalopathies, genetic therapeutic approaches capable of precisely targeting common pathological mechanisms could open up avenues for these devastating syndromes and more common types of epilepsy. With large-scale changes in brain networks during early disease onset, it would be imperative to develop effective therapies in neonatal or even prenatal stages to address these disorders [13].
In a cohort study published in 2023, involving 522 children with unexplained pediatric-onset epilepsy, exome sequencing was performed on patients and biological parents, and sequencing data were analyzed to detect single nucleotide variants (SNVs) and copy number variants (CNVs). The pathogenicity of the variants was assessed, patients were provided with their diagnostic results, and clinical utility was evaluated. Diagnostic findings included variants categorized as pathogenic, likely pathogenic (LP), or variants of uncertain significance (VUS) with clinical features consistent with the associated phenotype of the involved gene. Evidence of impact on a change in treatment or prognosis was observed. Genetic diagnosis led to discussion or actual change in treatment, including alteration in anticonvulsant medication or implementation of the ketogenic diet, in 27 patients (38%). Other management changes included referrals to other specialties due to the risk of non-neurological manifestations and withdrawal of anticonvulsant medication after genetic diagnosis suggested a self-resolving epilepsy (e.g., PRRT2). Five patients (7%) had a surprising change in prognosis, including early and unsuspected diagnosis of neuronal ceroid lipofuscinosis (CLN8). Genetic counseling, including counseling on reproductive risks, was offered to all families. It was particularly relevant for families with inherited variants and for both unaffected parents with low-level mosaic variants [14].
Advancements in genomics are expanding our understanding of epilepsy and have the potential to influence clinical treatment, prognosis, and patient counseling. Childhood-onset epilepsy has been observed to have a heterogeneous genetic basis, and some patients who previously lacked an explanation for their condition can now receive genetic diagnoses that have direct implications for their clinical care.
This advancement in achieving precise diagnoses has generated increasing interest in precision medicine for epilepsies, as it represents a benefit for patients and their families. A specific genetic diagnosis can provide important information about targeted treatment (pharmacogenomics), monitoring, prognosis, risk of recurrence, and establish a significant genotype/phenotype correlation important for reverse phenotyping and implementation of precision medicine.
Authors' Contribution
JMMF - information search, topic review, writing, editing, submission.
LJMG - writing, editing and final revision of the manuscript
References
Zweier M et al, La agrupación espacial de variantes de novo en CYFIP2, que codifica la proteína 2 que interactúa con FMRP citoplasmática, causa discapacidad intelectual y convulsiones. Eur J Hum Genet. mayo de 2019; 27(5):747-759. DOI: 10.1038/S41431-018-0331-Z. Epub 21 de enero de 2019. PMID: 30664714; PMCID: PMC6461771.
Biembengut, Í.V.; Shigunov, P.; Frota, N.F.; Lourenzoni, M.R.; de Souza, T.A.C.B. Dinámica molecular de la proteína CYFIP2 y su variante R87C relacionada con la encefalopatía epiléptica infantil temprana. Int. J. Mol. Sci. 2022, 23, 8708. https://doi.org/10.3390/ijms23158708
Cannabidiol Terapia exitosa para el desarrollo y la encefalopatía epiléptica relacionada con CYFIP2. Fernanda Veiga de Góes, Jessyca Thays Melo de Andrade Ramos, Rosiane da Silva Fontana, Cassio Luiz de Carvalho Serão, Fernando Kok, Dafne Dain Gandelman Horovitz. Revista Abierta de Neurología, 2022, Volumen 16. DOI: 10.2174/1874205X-v16-e2203290, 2022, 16, e1874205X2203290
Da Silva Cardoso J, Gomes R, Abreu M, et al. Papel clínico del codón 87 del gen CYFIP2 en la encefalopatía epiléptica infantil temprana: descripción de un caso clínico. Cureo 15(2). DOI 10.7759/cureus.35323 febrero, 2023
Encefalopatías epilépticas y del desarrollo: de la heterogeneidad genética al continuo fenotípico, Guerrini et al, Physiol Rev 103: 433–513, The American Physiological Society, 2023
Zhang Y, Lee Y, Han K. Función neuronal y disfunción de CYFIP2: de la dinámica de la actina a la encefalopatía epiléptica infantil temprana. BMB Rep. 2019 Mayo; 52(5):304-311. doi: 10.5483/BMBRep.2019.52.5.097. PMID: 30982501; PMCID: PMC6549915.
Begemann, A., Sticht, H., Begtrup, A. et al. Nuevos conocimientos sobre el espectro clínico y molecular del nuevo trastorno del neurodesarrollo relacionado con CYFIP2 y el deterioro de la dinámica de la actina mediada por WRC. Genet Med 23, 543–554 (2021). https://doi.org/10.1038/s41436-020-01011-x
Da Silva Cardoso J, Gomes R, Abreu M, et al. (22 de febrero de 2023) Papel clínico del codón 87 del gen CYFIP2 en la encefalopatía epiléptica infantil temprana: descripción de un caso clínico. Cureus 15(2): e35323. DOI 10.7759/cureus.35323
Cannabidiol Terapia exitosa para el desarrollo y la encefalopatía epiléptica relacionada con CYFIP2. Fernanda Veiga de Góes, Jessyca Thays Melo de Andrade Ramos, Rosiane da Silva Fontana, Cassio Luiz de Carvalho Serão, Fernando Kok, Dafne Dain Gandelman Horovitz. Revista Abierta de Neurología, 2022, Volumen 16. DOI: 10.2174/1874205X-v16-e2203290, 2022, 16, e1874205X2203290
Avances hacia terapias de precisión para las encefalopatías epilépticas y del desarrollo. Ilaria Bertocchi, Marco Cambiaghi, Mazahir T. Hasan, Frente. Neurosci., 06 de abril de 2023 Sec. Neurodesarrollo Volumen 17, 2023
Bartolini E. Encefalopatías epilépticas y del desarrollo hereditarias. Neurol Int. 3 de noviembre de 2021; 13(4):555-568. doi: 10.3390/neurolint13040055. PMID: 34842787; PMCID: PMC8628919.
Avances hacia terapias de precisión para las encefalopatías epilépticas y del desarrollo. Ilaria Bertocchi, Marco Cambiaghi, Mazahir T. Hasan, Frente. Neurosci., 06 de abril de 2023 Sec. Neurodesarrollo Volumen 17, 2023
Koh HY, Smith L, Wiltrout KN, et al. Utilidad de la secuenciación del exoma para el diagnóstico de la epilepsia de inicio pediátrico inexplicada. JAMA Netw Open. 2023; 6(7):E2324380. doi:10.1001/jamanetworkopen.2023.24380
Syrbe S. Encefalopatías epilépticas y del desarrollo: consecuencias terapéuticas de las pruebas genéticas. Medizinische genetik. 2022; 34(3): 215 224. https://doi.org/10.1515/medgen-2022-2145
suscripcion
issnes
eISSN L 3072-9610 (English)
Information
Use of data and Privacy - Digital Adversiting
Infomedic International 2006-2025.

